What Does Low Carb Do to Your Bones?

camtosh
Posts: 898 Member
What Does Low Carb Do to Your Bones?
posted 23 minutes ago by Dr. Andreas Eenfeldt in Low Carb High Fat, Myths about LCHF, New Study
What does low carb do to your bones? There is a lingering idea that eating low carb could result in osteoporosis, due to making blood acidic and leeching minerals from the bones.
However this theory has a few problems. For example, under normal circumstances the pH of the blood does not change depending on what diet you eat. The blood pH is tightly controlled within a very narrow span – or we’d die.
Testing the theory
More importantly this idea has been tested several times. A newly published study found the same thing as two earlier studies.
All three studies told a group of people to go on a strict low-carb diet (below 20 grams a day) and followed them for up to two years, comparing the results to a group on a high-carb diet.
Whether tracking markers of bone loss, or checking the bones with radiological methods (DEXA scans), the results were the same every time. Guess what?
Zero difference between the groups. Nothing happened to bone strength.
http://www.dietdoctor.com/low-carb-bone-health
Just posted online, thought we would like to read it here...
posted 23 minutes ago by Dr. Andreas Eenfeldt in Low Carb High Fat, Myths about LCHF, New Study
What does low carb do to your bones? There is a lingering idea that eating low carb could result in osteoporosis, due to making blood acidic and leeching minerals from the bones.
However this theory has a few problems. For example, under normal circumstances the pH of the blood does not change depending on what diet you eat. The blood pH is tightly controlled within a very narrow span – or we’d die.
Testing the theory
More importantly this idea has been tested several times. A newly published study found the same thing as two earlier studies.
All three studies told a group of people to go on a strict low-carb diet (below 20 grams a day) and followed them for up to two years, comparing the results to a group on a high-carb diet.
Whether tracking markers of bone loss, or checking the bones with radiological methods (DEXA scans), the results were the same every time. Guess what?
Zero difference between the groups. Nothing happened to bone strength.
http://www.dietdoctor.com/low-carb-bone-health
Just posted online, thought we would like to read it here...
0
Replies
-
Good to know. I think the idea originated with some old-school ketogenic diets for epilepsy. Those weren't very well formulated.
A recent study on rats confirmed that there could be a problem, but it was associated with low IGF-1 and growth hormone on a low-carb low-protein diet (similar to the old school ketogenic diets).
So my guess would be that if there is an issue it'd be due to too little protein rather than ketone-induced blood acidity.
Interestingly, a lot of people WANT the low IGF and GH environment because it's also thought to reduce cancer tumor growth.0 -
Interestingly, a lot of people WANT the low IGF and GH environment because it's also thought to reduce cancer tumor growth.
http://mybraincancerstory.blogspot.com/ <- Andrew's been working a bunch with researchers on that theory (he restricts protein)However this theory has a few problems. For example, under normal circumstances the pH of the blood does not change depending on what diet you eat. The blood pH is tightly controlled within a very narrow span – or we’d die.
I was just listening to a podcast that talked about this. Blood acidity is affected more by how we breathe, because we exhale the compounds that change the blood acidity level. If you stop breathing, or you hyperventilate, one of the reasons you pass out is because your blood pH goes beyond the upper or lower threshold (or reaches the edge of it). Food doesn't affect it.0 -
Well, food has an effect but it's buffered.
https://en.wikipedia.org/wiki/Bicarbonate_buffer_system
We can exhaust the buffering capacity, and that's what happens in ketoacidosis.
0 -
Fair enough. I should have said it doesn't have as much effect (breathing more directly affects it).0
-
Agreed, but I still wonder if some of us don't exhaust the buffer with ketone production.
http://emedicine.medscape.com/article/118361-workup
Levels greater than 0.5 mmol/L are considered abnormal, and levels of 3 mmol/L correlate with the need for treatment for DKA
At lot of abnormals around here. 0
0 -
Agreed, but I still wonder if some of us don't exhaust the buffer with ketone production.
http://emedicine.medscape.com/article/118361-workup
Levels greater than 0.5 mmol/L are considered abnormal, and levels of 3 mmol/L correlate with the need for treatment for DKA
At lot of abnormals around here.
o.O First impression is that those who are saying 3mmol/L = start treating for DKA are people who see people at the beginning of DKA... Now, that's a good thing that their Diabetic patients are getting caught that early, but insulin production counters ketone production and keeps people with insulin from going much beyond 3mmol...
A deeper looks shows that it's in the context of diabetics (the reference is to diabetics suffering DKA, though I can't see anything beyond the title from the link at the moment).
@Sunny_Bunny_ you've been neck-deep in this stuff lately. Thoughts?0 -
The point isn't really about the definition of DKA or when it should be treated, but that ketones at relatively low levels (i.e., not astronomically high levels) start affecting blood pH by exhausting the bicarbonate buffer.
If blood pH is affected long term, I can imagine some mineral leaching effects.
While definitions vary, mild DKA can be categorized by a pH level of 7.25-7.3 and a serum bicarbonate level between 15-18 mEq/L; moderate DKA can be categorized by a pH between 7.0-7.24 and a serum bicarbonate level of 10 to less than 15 mEq/L; and severe DKA has a pH less than 7.0 and bicarbonate less than 10 mEq/L.[12] In mild DKA, anion gap is greater than 10 and in moderate or severe DKA the anion gap is greater than 12. These figures differentiate DKA from HHS where blood glucose is greater than 600 mg/dL but pH is greater than 7.3 and serum bicarbonate greater than 15 mEq/L.0 -
Emily's respiration significantly increases with blood sugar for sure. I can actually tell based on her degree of panting, how far DKA has progressed. She literally pants like a tired dog.
I think a DKA diagnosis is given out a bit too often just because blood sugar is high and the person is suffering the effects of that alone in many cases where insulin production is still there.
Actual DKA is terrifying! Imagine a person that appears to be incredibly drunk. They can barely speak, can't hold their head steady, can't hold their eyes open, can't walk unassisted, in terrible pain and panting like a rabbid animal. That's what DKA looks like.
Like so many other things diabetes related, lumping the different forms together as if they are the same disease, creates confusion about what can actually occur in one patient compared to another. I think that is associated with some of the DKA diagnoses that simply are not.
I know that the panting is related to the acidity to some degree as well as it serving the purpose of releasing ketones.
As far as all the cool, blood data, I can access hers from past hospitalizations. I've looked over them in the past, but didn't understand the information like I would now. I'll try to do that while I'm sitting in school pick up line. 0
0 -
The point isn't really about the definition of DKA or when it should be treated, but that ketones at relatively low levels (i.e., not astronomically high levels) start affecting blood pH by exhausting the bicarbonate buffer.
If blood pH is affected long term, I can imagine some mineral leaching effects.
While definitions vary, mild DKA can be categorized by a pH level of 7.25-7.3 and a serum bicarbonate level between 15-18 mEq/L; moderate DKA can be categorized by a pH between 7.0-7.24 and a serum bicarbonate level of 10 to less than 15 mEq/L; and severe DKA has a pH less than 7.0 and bicarbonate less than 10 mEq/L.[12] In mild DKA, anion gap is greater than 10 and in moderate or severe DKA the anion gap is greater than 12. These figures differentiate DKA from HHS where blood glucose is greater than 600 mg/dL but pH is greater than 7.3 and serum bicarbonate greater than 15 mEq/L.
I missed that part somehow.
I think the question that needs to be addressed is whether the same changes happen to the buffer in nutritional ketosis in an otherwise healthy person (or at least in a person with normal blood sugar). DKA is, by its nature, a dysfunctional, uncontrolled state with not only elevated ketones, but also elevated blood sugar, whereas NK is functional and controlled, with normal blood sugar. While sugar doesn't affect pH level, I think it would be interesting to see what NK does to that buffer and whether the more controlled state actually needs the buffer (or if ketone production is also regulated by blood acidity, which would explain why it becomes increasingly difficult to produce more ketones after about 1-1.5mmol, and the 3+mmol range, according to Volek, generally only happens after exercise and isn't ideal as a chronic state).0 -
So, if you're interested in actual blood work that was taken during DKA, I have these in order of when they were taken. I left out a bunch of blood sugar checks because they were pretty stable once it came down the first night. There was a major spike the next day, but I'll have to get those results together still.
But here is day one. She was admitted around 5pm. So all of these tests happened in the evening of 1/15.








She had a basic metabolic panel done since going low carb and while not in DKA. But, even though she has been as low as 10-15g carbs some days, she has not tested positive for urine ketones at all. I think the basal insulin is preventing it. I'll go grab a capture of that panel. Maybe there's still some interesting information to be able to compare DKA to low carb...0 -
It was actually a comprehensive panel.
This was done since going Keto level low carb even though there have never been any positive ketone tests.
This was done on the doctor visit for the insulin oedema issue she has been having. So, that was going on hard core at the time. Only slightly better even now...
0 -
Interesting data, @Sunny_Bunny_! Too bad they didn't measure ketones.
By the pH metric, she had mild DKA.
By the HCO3 metric, it was moderate.
And by the anion gap metric, it was severe!
I hope she's feeling better!0 -
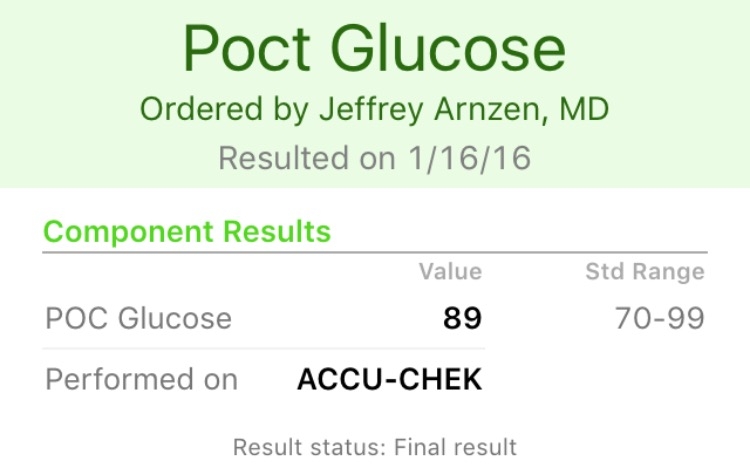
There's a whole day of testing on 1/16 and there's at least one ketone test that day that I recall. I was going to put together the tests from that day too.Interesting data, @Sunny_Bunny_! Too bad they didn't measure ketones.
By the pH metric, she had mild DKA.
By the HCO3 metric, it was moderate.
And by the anion gap metric, it was severe!
I hope she's feeling better!
She had a blood sugar spike back up on the 16th to around 500, for no identifiable reason since she was on IV insulin and not allowed food.
Yeah, isn't it weird how it doesn't necessarily reflect the same level of severity?
The numbers change so much throughout the day too. The 16th provides a full 24 hours of tests since she was hospitalized the entire day. Wasn't released until the 17th.
0 -
Ok. So, there are a lot of tests for a full day. I was mistaken though, she was released the evening of the 16th. So this still represents only about 16 or so hours of testing. But, the numbers got back into a good enough range to go home with a RX for potassium.








Then, blood sugar shot up. Since I was mixed up about when she was released, I realize now she was eating by this time. From the hospital menu for diabetics, which is full of potato, pasta, bread and fruit choices. You just can't get juice or regular soda. But she mostly stayed clear of those things. I can't remember what she ate, but it did a number on her bg.












Edited to put images in correct order.0
This discussion has been closed.


