Welcome to Debate Club! Please be aware that this is a space for respectful debate, and that your ideas will be challenged here. Please remember to critique the argument, not the author.
Anti-inflammatory foods
Options
Replies
-
NO night shade plants. This includes potatoes, tomatoes, egg plant and peppers (both red and green). I was diagnosed with RA 16 years ago and was on a multitude of prescriptions. After a couple of years with success in keeping my RA symptoms at bay I opted for a more holistic approach. This decision was reached because although my RA symptoms were not present...for the most part, an increase in the enzymes in my liver scared me. That increase was a direct result of just ONE of the medications I was on. I did much google research and read what I thought was yet another crack pot article on RA and night shade plants. After removing night shades from my diet, I have been completely free from prescriptions for over 12 years. I saw my RA doctor for my annual check up this month and all of my blood work was pretty much normal. I have slight levels of inflammation but he does not see the need for any prescriptions. This change in diet along with exercising has kept me flare up free for over 12 years. Is that enough science for you?
P.S. When I was diagnosed 16 years. I was diagnosed as severe. I could not walk down stairs or even stand for more then 5 minutes at a time. My knuckles in my hands were blue, I had rheumatoid nodules on my elbow and on my wrist. My range of motion was extremely limited. My RA doctor saw a wheelchair in my very near future. Now I walk/jog 4-8 miles a day.0 -
Wahl's Protocol looks into adding nutrient dense foods while avoiding inflammatory foods, mainly sugars, grains, dairy and starches, to treat autoimmune issues like MS. It's a paleo style diet which appears to be bordering on low carb or is low carb.
I think she was starting her own trials of the diet.
http://tedxtalks.ted.com/video/TEDxIowaCity-Dr-Terry-Wahls-Min
http://terrywahls.com/about-the-wahls-protocol/
A summary of her daily diet:
3 cups of cruciferous and dark greens
3 cups intensely coloured: 1 cup red vegetables / fruit, 1 cup blue black vegetables / fruits, 1 cup yellow/orange vegetable / fruits
3 cups others including: 1 cup mushrooms / onion family (for organic sulphur), and seaweed for iodine and trace minerals.
(Note: 1 cup = raw vegetables chopped = 1/2 cup cooked, an apple sized fruit, or 2 cups leafy greens)
Include spices and herbs.
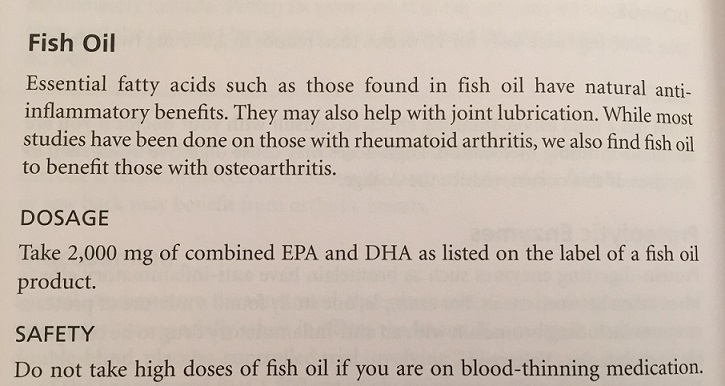
Omega 3 rich foods, green leaves and animals fed green leaves, wild fish and seafood. And you could add fish oil.
Eat organ meats once per week
Regular bone broth
Fermented foods or a probiotic
Ugh my body can't handle most of those foods. Crohn's and UC are odd where salad is one of the worst nutritional choices you can make. Some IBDers can handle it but just thinking about eating one gives me abdominal pain.0 -
KimDaniels2 wrote: »NO night shade plants. This includes potatoes, tomatoes, egg plant and peppers (both red and green). I was diagnosed with RA 16 years ago and was on a multitude of prescriptions. After a couple of years with success in keeping my RA symptoms at bay I opted for a more holistic approach. This decision was reached because although my RA symptoms were not present...for the most part, an increase in the enzymes in my liver scared me. That increase was a direct result of just ONE of the medications I was on. I did much google research and read what I thought was yet another crack pot article on RA and night shade plants. After removing night shades from my diet, I have been completely free from prescriptions for over 12 years. I saw my RA doctor for my annual check up this month and all of my blood work was pretty much normal. I have slight levels of inflammation but he does not see the need for any prescriptions. This change in diet along with exercising has kept me flare up free for over 12 years. Is that enough science for you???
I agree about the nightshades though sweet potatoes and potatoes are 2 of the 4 vegetables my body can handle and don't bother me that much. Tomatoes on the other hand are killer.0 -
This is all very interesting. I note (and again, sceptical of the page) that the Harvard page specifically lists tomatoes as a go-to anti-inflammatory food.0
-
-
-
Great article about nightshades and inflammation, with a long list of foods to avoid:
http://www.sott.net/article/261186-The-link-between-nightshades-chronic-pain-and-inflammation
0 -
singingflutelady wrote: »Looks interesting. Unfortunately I am classified as severe and probably will never get off my meds (I'm on Remicade-a biologic and azathioprine).We have a current study at our institution looking at using mangos to treat IBD. It's still way to early in the trial for results though.
https://clinicaltrials.gov/ct2/show/NCT02227602?term=Mango+ibd&rank=1
I would think that adding in some foods proven to reduce inflammation in ibd (again, don't know if there's any conclusive evidence) could help in addition to medication. Sorry to hear you have such a severe case, but hopefully you've found a regimen that works to keep your symptoms in check.0 -
Tomatoes should not be on an anti-inflammatory list without a boatload of caveats. I wonder if they put these lists together simply looking at things like "hey there are a ton of antioxidants in tomatoes so tomatoes must be awesome!", without taking into account things like the solanine in tomatoes, which can far outweigh the positive benefits of the antioxidants in people sensitive to its effects.0
-
It seems as if there's unlikely to be foods that are and are not inflammatory (and that it's not clear that it matters for most people). Instead, there are probably foods that interact with particular conditions or tendencies for inflammation, just as there are different reasons for inflammation (some problems, some not).0
-
KimDaniels2 wrote: »NO night shade plants. This includes potatoes, tomatoes, egg plant and peppers (both red and green). I was diagnosed with RA 16 years ago and was on a multitude of prescriptions. After a couple of years with success in keeping my RA symptoms at bay I opted for a more holistic approach. This decision was reached because although my RA symptoms were not present...for the most part, an increase in the enzymes in my liver scared me. That increase was a direct result of just ONE of the medications I was on. I did much google research and read what I thought was yet another crack pot article on RA and night shade plants. After removing night shades from my diet, I have been completely free from prescriptions for over 12 years. I saw my RA doctor for my annual check up this month and all of my blood work was pretty much normal. I have slight levels of inflammation but he does not see the need for any prescriptions. This change in diet along with exercising has kept me flare up free for over 12 years. Is that enough science for you?
P.S. When I was diagnosed 16 years. I was diagnosed as severe. I could not walk down stairs or even stand for more then 5 minutes at a time. My knuckles in my hands were blue, I had rheumatoid nodules on my elbow and on my wrist. My range of motion was extremely limited. My RA doctor saw a wheelchair in my very near future. Now I walk/jog 4-8 miles a day.
Thanks for posting this. I'm going to do a little experiment myself with tomatoes. I enjoy anecdotal evidence (especially compelling like this), and it is anecdotal evidence that spurs proper studies, so it has a place in science, but it's obviously inconclusive on its own. So when you say "Is that enough science for you?", well...
0 -
lemurcat12 wrote: »It seems as if there's unlikely to be foods that are and are not inflammatory (and that it's not clear that it matters for most people). Instead, there are probably foods that interact with particular conditions or tendencies for inflammation, just as there are different reasons for inflammation (some problems, some not).
I agree. Even if we were to stick to one problem (like RA) it seems like we'd have a tough go of it. But adding in different autoimmune disorders makes the discussion unwieldy. OP, is there a particular autoimmune disorder that you are concerned about?
0 -
In my opinion (and experience) a person doesnt necessarily hVe to eat certain foods to trigger inflammatory response. For example: you can eat 1,000 calories a day worth of inflammatory foods (lets say classic- sugary cake) and not experience inflammation. If same food in same person is upped to 2,000 calories- inflammation entails.culprit here is insulin response, which triggers inflammation. Read this article- very lengthy but totally worth it: http://articles.mercola.com/sites/articles/archive/2001/07/14/insulin-part-one.aspx
In addition, the body fat cells produce inflammation in themselves- so you can eat all organic, non gmo, pesticide free, etc etc, but as long as you are OVEReating and gaining body fat inflammation will persist. All this from experience and reading, reading, reading, reading what seems like hundreds of books, blogs, articles. Lastly, overeating keeps your liver too budy metabolising the food you consume instead of delotxing excess estrogens which are another source of inflammation.
In 3 yrs studying all this due to my own health problems I have come to conclusion that inflammation is 99% tied to overeating and excess body fat.1 -
I think there is a lot of truth to that, although I wouldn't say that all inflammation is due to excess body fat. Based on my health, I do agree with the role of insulin resistance and inflammation. The thing is though, I'm in a unique situation: I am insulin resistant but don't have any excess body fat. But I do think that there is definitely too much inflammation in my system, which is probably connected (maybe a chicken-and-egg scenario) to my insulin resistance. It wasn't overeating that got me in this situation, but probably a combination of other factors, including a diet high in carbs/gluten for many years.In my opinion (and experience) a person doesnt necessarily hVe to eat certain foods to trigger inflammatory response. For example: you can eat 1,000 calories a day worth of inflammatory foods (lets say classic- sugary cake) and not experience inflammation. If same food in same person is upped to 2,000 calories- inflammation entails.culprit here is insulin response, which triggers inflammation. Read this article- very lengthy but totally worth it: http://articles.mercola.com/sites/articles/archive/2001/07/14/insulin-part-one.aspx
In addition, the body fat cells produce inflammation in themselves- so you can eat all organic, non gmo, pesticide free, etc etc, but as long as you are OVEReating and gaining body fat inflammation will persist. All this from experience and reading, reading, reading, reading what seems like hundreds of books, blogs, articles. Lastly, overeating keeps your liver too budy metabolising the food you consume instead of delotxing excess estrogens which are another source of inflammation.
In 3 yrs studying all this due to my own health problems I have come to conclusion that inflammation is 99% tied to overeating and excess body fat.
0 -
ForecasterJason wrote: »
I think there is a lot of truth to that, although I wouldn't say that all inflammation is due to excess body fat. Based on my health, I do agree with the role of insulin resistance and inflammation. The thing is though, I'm in a unique situation: I am insulin resistant but don't have any excess body fat. But I do think that there is definitely too much inflammation in my system, which is probably connected (maybe a chicken-and-egg scenario) to my insulin resistance. It wasn't overeating that got me in this situation, but probably a combination of other factors, including a diet high in carbs/gluten for many years.In my opinion (and experience) a person doesnt necessarily hVe to eat certain foods to trigger inflammatory response. For example: you can eat 1,000 calories a day worth of inflammatory foods (lets say classic- sugary cake) and not experience inflammation. If same food in same person is upped to 2,000 calories- inflammation entails.culprit here is insulin response, which triggers inflammation. Read this article- very lengthy but totally worth it: http://articles.mercola.com/sites/articles/archive/2001/07/14/insulin-part-one.aspx
In addition, the body fat cells produce inflammation in themselves- so you can eat all organic, non gmo, pesticide free, etc etc, but as long as you are OVEReating and gaining body fat inflammation will persist. All this from experience and reading, reading, reading, reading what seems like hundreds of books, blogs, articles. Lastly, overeating keeps your liver too budy metabolising the food you consume instead of delotxing excess estrogens which are another source of inflammation.
In 3 yrs studying all this due to my own health problems I have come to conclusion that inflammation is 99% tied to overeating and excess body fat.
What is the "inflammation" that you are talking about, and why do you think it's the cause of your issues? There's a specific meaning for something like autoimmune diseases, so obviously I am not talking about those, but it gets thrown around like a buzz word these days, especially by the Mercolas of the world.
0 -
We also have a lot of studies going on looking at the role of inflammation and mod disorders (mainly major depressive disorder and generalized depression). I'm not sure they know why, but they're seeing increased expression and protein levels of inflammatory markers in those populations.
I need to read up on it, but I believe so far they are just correlation studies.0 -
Turmeric or Curcumin is great imo. I currently take it as a supplement daily. Turmeric aborbs best with pepper (so add a peppercorn!)0
-
I've had some IBS symptoms for a long time, and it seems to me that something (or multiple foods) I'm eating are inflaming my gut (I'm trying to do the best I can to help manage this while keeping my calorie intake up). Most nights, my sleep quality is not the greatest (despite doing almost everything right when it comes to sleep hygiene), and I think it is related to gut inflammation. The poorer my sleep is on a given night, the more aroused my digestive system is in the morning (and vice-versa). I also find that my mood tends to take a hit whenever my digestive system is a bit more aroused than normal. I know there is a stress component to all of this, which from my understanding is enhancing the inflammatory response. I have noticed over the past few years that my best nights of sleep have come when I am both "extra" relaxed and my digestion has been good.lemurcat12 wrote: »ForecasterJason wrote: »
I think there is a lot of truth to that, although I wouldn't say that all inflammation is due to excess body fat. Based on my health, I do agree with the role of insulin resistance and inflammation. The thing is though, I'm in a unique situation: I am insulin resistant but don't have any excess body fat. But I do think that there is definitely too much inflammation in my system, which is probably connected (maybe a chicken-and-egg scenario) to my insulin resistance. It wasn't overeating that got me in this situation, but probably a combination of other factors, including a diet high in carbs/gluten for many years.In my opinion (and experience) a person doesnt necessarily hVe to eat certain foods to trigger inflammatory response. For example: you can eat 1,000 calories a day worth of inflammatory foods (lets say classic- sugary cake) and not experience inflammation. If same food in same person is upped to 2,000 calories- inflammation entails.culprit here is insulin response, which triggers inflammation. Read this article- very lengthy but totally worth it: http://articles.mercola.com/sites/articles/archive/2001/07/14/insulin-part-one.aspx
In addition, the body fat cells produce inflammation in themselves- so you can eat all organic, non gmo, pesticide free, etc etc, but as long as you are OVEReating and gaining body fat inflammation will persist. All this from experience and reading, reading, reading, reading what seems like hundreds of books, blogs, articles. Lastly, overeating keeps your liver too budy metabolising the food you consume instead of delotxing excess estrogens which are another source of inflammation.
In 3 yrs studying all this due to my own health problems I have come to conclusion that inflammation is 99% tied to overeating and excess body fat.
What is the "inflammation" that you are talking about, and why do you think it's the cause of your issues? There's a specific meaning for something like autoimmune diseases, so obviously I am not talking about those, but it gets thrown around like a buzz word these days, especially by the Mercolas of the world.
I suspect a lot of this is could be driven an imbalance of serotonin and cortisol. Physically, over the last few years I've felt best in the late spring/early summer, which could be explained by seasonal changes in serotonin. Over the last few months I've found some articles that go into the science behind how gut health is implicated in sleep and inflammation. Basically, if something is disturbing the gut, it can send inflammatory signals throughout the body.
http://gutcritters.com/why-cant-i-sleep-part-two-leaky-gut-endotoxemia-and-inflammation/
https://doctordoni.com/2015/01/how-inflammation-and-pain-affect-your-sleep.html0 -
lemurcat12 wrote: »ForecasterJason wrote: »
I think there is a lot of truth to that, although I wouldn't say that all inflammation is due to excess body fat. Based on my health, I do agree with the role of insulin resistance and inflammation. The thing is though, I'm in a unique situation: I am insulin resistant but don't have any excess body fat. But I do think that there is definitely too much inflammation in my system, which is probably connected (maybe a chicken-and-egg scenario) to my insulin resistance. It wasn't overeating that got me in this situation, but probably a combination of other factors, including a diet high in carbs/gluten for many years.In my opinion (and experience) a person doesnt necessarily hVe to eat certain foods to trigger inflammatory response. For example: you can eat 1,000 calories a day worth of inflammatory foods (lets say classic- sugary cake) and not experience inflammation. If same food in same person is upped to 2,000 calories- inflammation entails.culprit here is insulin response, which triggers inflammation. Read this article- very lengthy but totally worth it: http://articles.mercola.com/sites/articles/archive/2001/07/14/insulin-part-one.aspx
In addition, the body fat cells produce inflammation in themselves- so you can eat all organic, non gmo, pesticide free, etc etc, but as long as you are OVEReating and gaining body fat inflammation will persist. All this from experience and reading, reading, reading, reading what seems like hundreds of books, blogs, articles. Lastly, overeating keeps your liver too budy metabolising the food you consume instead of delotxing excess estrogens which are another source of inflammation.
In 3 yrs studying all this due to my own health problems I have come to conclusion that inflammation is 99% tied to overeating and excess body fat.
What is the "inflammation" that you are talking about, and why do you think it's the cause of your issues? There's a specific meaning for something like autoimmune diseases, so obviously I am not talking about those, but it gets thrown around like a buzz word these days, especially by the Mercolas of the world.
Ugh. Quackery at its worst.0 -
ForecasterJason wrote: »
I've had some IBS symptoms for a long time, and it seems to me that something (or multiple foods) I'm eating are inflaming my gut (I'm trying to do the best I can to help manage this while keeping my calorie intake up).lemurcat12 wrote: »ForecasterJason wrote: »
I think there is a lot of truth to that, although I wouldn't say that all inflammation is due to excess body fat. Based on my health, I do agree with the role of insulin resistance and inflammation. The thing is though, I'm in a unique situation: I am insulin resistant but don't have any excess body fat. But I do think that there is definitely too much inflammation in my system, which is probably connected (maybe a chicken-and-egg scenario) to my insulin resistance. It wasn't overeating that got me in this situation, but probably a combination of other factors, including a diet high in carbs/gluten for many years.In my opinion (and experience) a person doesnt necessarily hVe to eat certain foods to trigger inflammatory response. For example: you can eat 1,000 calories a day worth of inflammatory foods (lets say classic- sugary cake) and not experience inflammation. If same food in same person is upped to 2,000 calories- inflammation entails.culprit here is insulin response, which triggers inflammation. Read this article- very lengthy but totally worth it: http://articles.mercola.com/sites/articles/archive/2001/07/14/insulin-part-one.aspx
In addition, the body fat cells produce inflammation in themselves- so you can eat all organic, non gmo, pesticide free, etc etc, but as long as you are OVEReating and gaining body fat inflammation will persist. All this from experience and reading, reading, reading, reading what seems like hundreds of books, blogs, articles. Lastly, overeating keeps your liver too budy metabolising the food you consume instead of delotxing excess estrogens which are another source of inflammation.
In 3 yrs studying all this due to my own health problems I have come to conclusion that inflammation is 99% tied to overeating and excess body fat.
What is the "inflammation" that you are talking about, and why do you think it's the cause of your issues? There's a specific meaning for something like autoimmune diseases, so obviously I am not talking about those, but it gets thrown around like a buzz word these days, especially by the Mercolas of the world.
This sounds like the kind of self-diagnosis that raises my skepticism, especially when it falls into the trendy explanation of the day. I'd work with a doctor (not a naturopath) and try and get an explanation if having a digestive issue (which I wouldn't assume is about "inflammation" or "leaky gut" which to my understanding has yet to be proven to be a real thing).0 -
I understand the skepticism, but new research is showing that inflammation is involved in IBS. I would think the question is why is it the case.This study talks about inflammation and IBS. "There is increasing evidence of the presence of low grade inflammation in the intestinal mucosa of patients with IBS but the mechanisms involved in this process are by no means fully understood." Here is another study. "It is becoming increasingly clear that inflammation of the intestinal mucosa and nerves causes the altered GI dysfunction seen in IBS."lemurcat12 wrote: »ForecasterJason wrote: »
I've had some IBS symptoms for a long time, and it seems to me that something (or multiple foods) I'm eating are inflaming my gut (I'm trying to do the best I can to help manage this while keeping my calorie intake up).lemurcat12 wrote: »ForecasterJason wrote: »
I think there is a lot of truth to that, although I wouldn't say that all inflammation is due to excess body fat. Based on my health, I do agree with the role of insulin resistance and inflammation. The thing is though, I'm in a unique situation: I am insulin resistant but don't have any excess body fat. But I do think that there is definitely too much inflammation in my system, which is probably connected (maybe a chicken-and-egg scenario) to my insulin resistance. It wasn't overeating that got me in this situation, but probably a combination of other factors, including a diet high in carbs/gluten for many years.In my opinion (and experience) a person doesnt necessarily hVe to eat certain foods to trigger inflammatory response. For example: you can eat 1,000 calories a day worth of inflammatory foods (lets say classic- sugary cake) and not experience inflammation. If same food in same person is upped to 2,000 calories- inflammation entails.culprit here is insulin response, which triggers inflammation. Read this article- very lengthy but totally worth it: http://articles.mercola.com/sites/articles/archive/2001/07/14/insulin-part-one.aspx
In addition, the body fat cells produce inflammation in themselves- so you can eat all organic, non gmo, pesticide free, etc etc, but as long as you are OVEReating and gaining body fat inflammation will persist. All this from experience and reading, reading, reading, reading what seems like hundreds of books, blogs, articles. Lastly, overeating keeps your liver too budy metabolising the food you consume instead of delotxing excess estrogens which are another source of inflammation.
In 3 yrs studying all this due to my own health problems I have come to conclusion that inflammation is 99% tied to overeating and excess body fat.
What is the "inflammation" that you are talking about, and why do you think it's the cause of your issues? There's a specific meaning for something like autoimmune diseases, so obviously I am not talking about those, but it gets thrown around like a buzz word these days, especially by the Mercolas of the world.
This sounds like the kind of self-diagnosis that raises my skepticism, especially when it falls into the trendy explanation of the day. I'd work with a doctor (not a naturopath) and try and get an explanation if having a digestive issue (which I wouldn't assume is about "inflammation" or "leaky gut" which to my understanding has yet to be proven to be a real thing).
(Note the difference in wording along with the difference in year publication between those two studies.)
0 -
In my opinion (and experience) a person doesnt necessarily hVe to eat certain foods to trigger inflammatory response. For example: you can eat 1,000 calories a day worth of inflammatory foods (lets say classic- sugary cake) and not experience inflammation. If same food in same person is upped to 2,000 calories- inflammation entails.culprit here is insulin response, which triggers inflammation. Read this article- very lengthy but totally worth it: http://articles.mercola.com/sites/articles/archive/2001/07/14/insulin-part-one.aspx
In addition, the body fat cells produce inflammation in themselves- so you can eat all organic, non gmo, pesticide free, etc etc, but as long as you are OVEReating and gaining body fat inflammation will persist. All this from experience and reading, reading, reading, reading what seems like hundreds of books, blogs, articles. Lastly, overeating keeps your liver too budy metabolising the food you consume instead of delotxing excess estrogens which are another source of inflammation.
In 3 yrs studying all this due to my own health problems I have come to conclusion that inflammation is 99% tied to overeating and excess body fat.
The only impact GMO status of food should have on inflammation would be eating the experimental plants altered to produce EPA and DHA in their oils.0 -
We also have a lot of studies going on looking at the role of inflammation and mod disorders (mainly major depressive disorder and generalized depression). I'm not sure they know why, but they're seeing increased expression and protein levels of inflammatory markers in those populations.
I need to read up on it, but I believe so far they are just correlation studies.
I would hypothesize it has to with cortisol / glucocorticoids. Depression and the stress response means that people suffering from it often have high levels of glucocorticoids that are typically anti-inflammatory and lower the body's immune response. The result of prolonged excess shut off might be that the body believes it is receiving a false signal and therefore upgregulates other pro-inflammatory activity.
I'm inclined to believe that more than the idea that depression is the body fighting what is a person with naturally high levels of pro-inflammatory metabolism, but that's another possibility.0 -
Hope you don't mind me adding in my experience with all this. I have been diagnosed with Lupus for about 3 years now but seriously suspect that it was affecting me long before the official stamp was given, alongside that I have had CRPS 1 since 1997 and that seems to be affecting my organs such as gut, liver and kidneys all confirmed by blood testing, colonoscopy and endoscopy. It is all very complicated as the Lupus is severe and it has done a number on my kidneys as well.....so where one begins and another starts is very cloudy.
I have ulcerative colitis as well and this started not long after the CRPS diagnosis (perhaps related) and this lead me down the path of trying to eliminate any offending dietary impacts I could.
For me living the life I do now with all the inflammation and pain of the 2 issues my diet has undergone a radical shift.
I had a look at the list @jgnatca kindly put up and I have found that for me the list pretty much rings true and I have had good results with the 'friendly' foods and bad reactions to the 'inflammatory' ones.
I cannot tolerate nightshades at all with the exception of limited quantities of fresh tomatoes. Eggplant, mushrooms, capsicums and particularly potatoes all cause intense joint pain and gastric distress. We use pumpkin with little problem instead.
Dairy is an interesting one. I can manage small amounts of cheese, homemade plain greek yoghurt and lactose free milk, if I push my luck with normal milk, again it's a horrible crampy painful nightmare. I am reluctant though to eliminate these sources of calcium altogether as I have severe osteoporosis and have already broken my back once.
Soy in all it's forms is a no no and so are grains except for minimal, infrequent servings of rice. I'll put my hand up and say that wheat is RIGHT OUT. I want it, crave it even but it does me no favours, particularly processed sugary products are absolutely deadly for giving me pain and inflammation.
I've dabbled with IF as a way of combating the constant impact of dealing with foods in my system...someone up thread alluded to this concept. I did find my pain levels improved having a break from the 'load' of digesting and eliminating and often when things are truly nightmarish will resort to a short 24 hour fast to try to give my system a break. It works for me but I am no position to call it anything other than anecdotal.
TL:DR If you have an auto-immune condition or one that deals the cards of chronic pain, use yourself as an experiment. What foods work for you may be someone else's kryptonite. Also it's a good idea to keep a diary as it can all get very confusing.
All the best. Hope I haven't ramble too much and I have helped answer your query @Alatariel75
0 -
Ok, I will share some of my experiences after being diagnosed with ulcerative colitis almost 10 years ago and proctitis 6 years ago. First of all, I was not in a good place when I was diagnosed. My intestines looked like raw hamburger meat in my first colonoscopy ... everything, including water set me off. It was a long road back to health. Once I managed to leave the hospital after some heavy duty drugs (which made about 40% of my hair fall out), it was pretty much an experiment to what I could eat. Add the overall body inflammation and I was a walking hot mess of hurt. (Oh and by the way, ALL of the inflammation markers in my bloodwork appeared NORMAL which is why my condition went undiagnosed for so long ... it had to be in my mind because the bloodwork doesn't lie does it? I had to pay for my colonoscopy out of pocket because insurance would not because the doctors (all 3 of them I tried) said it was in my head ... before it was all over, two of the three came to my hospital room and apologized.)
Dairy you purchase in the store was out. However, raw goats milk was a godsend for me and one of the most soothing things I could tolerate after my hospital stay. Luckily, my in-laws were raising goats at the time so I had a steady supply. Fresh cherries and fresh pineapple were two biggies in my anti-inflammatory diet and worked wonders for me. REd and purple grapes were good but not the green ones. My gut liked kiwis but hated bananas. I was introduced to fermented foods which helped repopulate my gut with good bacteria and was another great soother.
Most nightshades were not a problem for me and did not exacerbate my inflammation but I still kept them to a minimum for the first year of healing. I tried to go gluten-free but I just could not sustain it so I just avoided all wheat products because it caused pain and bloating. However, I got brave and tried some bread my mother in law made from wheat that she ground herself. She bought the entire wheatberry from an organic, heritage wheat source and ground her own flour. THAT I could handle so now when I bake, I use that flour instead of the bleached sanitized version stripped of all nutrients that you buy in the supermarket.
I also upped my fat intake, specifically wild-caught salmon and mackerel, organic chicken with the skin kept on, added coconut oil in various ways to my diet and started making my own salad dressing with olive oil. And no fried foods!
Fast forward to now and my UC and proctitis is in remission and I still keep as many anti-inflammatory foods in my diet as possible. However, I still have some body inflammation which makes working out a pain (literally). However, overall body aches I can tolerate because the exercise and weight lifting helped me lose the weight I needed to lose which made my overall health better. However, my doctor (one that finally diagnosed me and believed in me) cannot explain my constant low level of inflammation. I have a feeling that one of these days I will buckle down and remove all grains and see what happens. Right now, I just don't want to do so because that would mean no more rice, oats, farrow and anything made with wheat, etc. The doctor doesn't think it will help but so many others I have met in person and online that have quit grains have reported alleviation of symptoms. I guess when I get to the point that I cannot tolerate it anymore, I will try but for now, I deal.0 -
Inflammation as is mentioned when eating food doesn't have to mean stuff you see. There are disorders in the cardiovascular system that can be attributed to inflammation, and you'd never know it. I don't have the details on that stuff though.
Since people want science, I'd recommend not using a regular google search but instead use Google Scholar. There you can get links to the actual real studies instead of what others say to try and sell a product or website hits. You might not be able to get all articles without paying for them, because researchers and journals that do the publishing have to pay bills too. But, you might find something worth investigating further. Also, some of the reading may be difficult, but journalists who try to summarize the research often get it wrong as well because they aren't specialists in that field. They are specialists at writing. The only way to really check what's going on is to read the research.0 -
A PI in my department studies the effects of curcurmin (active component) in turmeric in the context of a couple of different cancers, colorectal is his main focus. He's branching out to other diseases.
Unfortunately, while curcurmin definitely has an anti-inflammatory effect both in vivo and in vitro (shown via microarray as a down-regulation of inflammatory pathway transcripts in blood and the tissue cultures tested), you don't get enough curcurmin from the amounts of turmeric eaten in food to do much of anything. Not even if you eat it at almost every meal.
If you take turmeric capsules as supplements, there is a real risk of toxicity from overdose of other components of turmeric. You can get curcurmin supplements. Those would be the better choice, but keep in mind that an anti-inflammatory response is not in all cases a good thing. Anti-inflammatories can also impede the body's ability to fight off disease - inflammation is part of that process.0 -
A PI in my department studies the effects of curcurmin (active component) in turmeric in the context of a couple of different cancers, colorectal is his main focus. He's branching out to other diseases.
Unfortunately, while curcurmin definitely has an anti-inflammatory effect both in vivo and in vitro (shown via microarray as a down-regulation of inflammatory pathway transcripts in blood and the tissue cultures tested), you don't get enough curcurmin from the amounts of turmeric eaten in food to do much of anything. Not even if you eat it at almost every meal.
If you take turmeric capsules as supplements, there is a real risk of toxicity from overdose of other components of turmeric. You can get curcurmin supplements. Those would be the better choice, but keep in mind that an anti-inflammatory response is not in all cases a good thing. Anti-inflammatories can also impede the body's ability to fight off disease - inflammation is part of that process.
I know the importance of inflammation but as I said earlier I have Crohn's disease so inflammation is a big problem for me. I will try curcurmin supplements.0 -
singingflutelady wrote: »A PI in my department studies the effects of curcurmin (active component) in turmeric in the context of a couple of different cancers, colorectal is his main focus. He's branching out to other diseases.
Unfortunately, while curcurmin definitely has an anti-inflammatory effect both in vivo and in vitro (shown via microarray as a down-regulation of inflammatory pathway transcripts in blood and the tissue cultures tested), you don't get enough curcurmin from the amounts of turmeric eaten in food to do much of anything. Not even if you eat it at almost every meal.
If you take turmeric capsules as supplements, there is a real risk of toxicity from overdose of other components of turmeric. You can get curcurmin supplements. Those would be the better choice, but keep in mind that an anti-inflammatory response is not in all cases a good thing. Anti-inflammatories can also impede the body's ability to fight off disease - inflammation is part of that process.
I know the importance of inflammation but as I said earlier I have Crohn's disease so inflammation is a big problem for me. I will try curcurmin supplements.
Here's a reference with a lot of information and links to numerous scientific studies: https://examine.com/supplements/curcumin/
(Examine.com is a good reference for most any nutrient/supplement you can think of. Definitely worth bookmarking.)0 -
Thanks.0
This discussion has been closed.
Categories
- All Categories
- 1.4M Health, Wellness and Goals
- 396.7K Introduce Yourself
- 44.2K Getting Started
- 260.8K Health and Weight Loss
- 176.3K Food and Nutrition
- 47.6K Recipes
- 232.8K Fitness and Exercise
- 450 Sleep, Mindfulness and Overall Wellness
- 6.5K Goal: Maintaining Weight
- 8.7K Goal: Gaining Weight and Body Building
- 153.3K Motivation and Support
- 8.3K Challenges
- 1.3K Debate Club
- 96.5K Chit-Chat
- 2.6K Fun and Games
- 4.5K MyFitnessPal Information
- 16 News and Announcements
- 18 MyFitnessPal Academy
- 1.4K Feature Suggestions and Ideas
- 3.1K MyFitnessPal Tech Support Questions